Procedure overview:
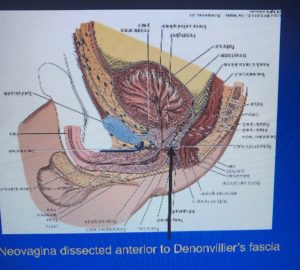
The first steps are to remove genital hair with electrolysis as this skin becomes the interior of the neovaginal canal. The skin of the penile shaft is inverted to form a vaginal cavity termed penile infundibulation. The glans is fashioned into a functional clitoris without disrupting the nerve and blood supply. The bulbar urethra is incised ventrally, and the dorsal aspect is used to form the anterior vaginal wall. Labia are formed from scrotal skin. Levator ani musculature are released to widen pelvic floor.
Sigmoid vaginoplasty is a rarer technique. This is used primarily for those with penoscrotal hypoplasia due to pubertal suppression from a young age, or for revisions. This technique has no limit to depth and may provide some endogenous lubrication due to sigmoid goblet cells; this lubrication can have positive and negative aspects for some folks as it may be constant/unspleasant and unrelated to sexual arousal.
Post surgical care (up to 8 weeks:)
The goal is 5 – 6.5 inches of vaginal depth as there is no muscularis layer for stretch. Skin or sigmoid grafts may be required to reach 5cm with hypoplasia or with circumcision. Ongoing dilation is required for maintenance of the vaginal cavity for at least one year, especially with penile inversion techniques.
New pleasurable sensations may take time – forcing your body to experience pleasure and pain at the same time by experimenting with clitoral sensation during dilation may not work for everyone. Give your body time to adjust to its new form and be creative with your touch and self care.
A second surgery/ labioplasty may be desired to adjust the labia majora, create a clitoral hood, define the labia minora and adjust urethral position.
Brownish yellow discharge is expected for up to 6 weeks after surgery. Bleeding and spotting may continue up to 8 weeks. The neovagina is made from epidermis; therefore, a mild lavender or chamomile soap and water douche is effective treatment. (UCSF SOC.) Use an organic cotton pad or panty liner during this time – available at Whole Foods or your local healthy store. They are less bulky, more breathable, feel nicer, and minimize plastic and chemical exposures.
Neovaginal Infundibulum: a microbiome of its own
 The epidermal neovaginal microbiome cannot be compared to the cisgender microbiome. Gram negative flora including proteus, gardnerella and enterococcus are common; few lactobacilli are present. The endogenous normal pH is 5.88 in the neovagina. Therefore, antibiotic treatment may be different from cisvaginal bacterial vaginosis as the microbiome is different for epidermal and sigmoid mucosa.
The epidermal neovaginal microbiome cannot be compared to the cisgender microbiome. Gram negative flora including proteus, gardnerella and enterococcus are common; few lactobacilli are present. The endogenous normal pH is 5.88 in the neovagina. Therefore, antibiotic treatment may be different from cisvaginal bacterial vaginosis as the microbiome is different for epidermal and sigmoid mucosa.
Discharge/Itching/Odor
 Because this type of neovagina is made of epidermal skin, it needs to be washed regularly. Mild soap and water douches are required 2-3 times per week to remove cellular debris, creams and/or lubricants. Gentle soaps without sodium laurel sulphate, artificial colors and scents, or harsh detergents are the least likely to result in irritation. Mild lavender or chamomile soaps have additional antimicrobial effects and are recommended by the UCSF Trans Health Guidelines. Body washes created for babies are often good low chemical choices.
Because this type of neovagina is made of epidermal skin, it needs to be washed regularly. Mild soap and water douches are required 2-3 times per week to remove cellular debris, creams and/or lubricants. Gentle soaps without sodium laurel sulphate, artificial colors and scents, or harsh detergents are the least likely to result in irritation. Mild lavender or chamomile soaps have additional antimicrobial effects and are recommended by the UCSF Trans Health Guidelines. Body washes created for babies are often good low chemical choices.
A white vinegar or 25% povidone-iodine solution may be used instead of soap for malodorous discharge. However, be cautious chronically treating without a thorough evaluation as discharge can be a sign that something needs medical attention. Use PCR to diagnose bacterial vaginosis and assess antibiotic sensitivities. Vaginal estrogen may also help maintain tissue softness and elasticity.
DDX: Discharge or bleeding in Infundibular neovagina
- Neovaginitis
- Malignancy
- Granulation tissue
- STI – test urethra as well as vaginal cavity
The Sigmoid Neovagina: a complex ecosystem
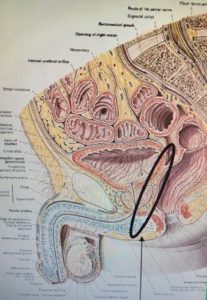 An apical cap of sigmoid tissue is an alternative laproscopic surgical procedure to create or lengthen a neovagina. The penile skin available is used for labia minora and ventral penile flaps form the meatus of the urethra. As colonic tissue is used, this vagina will have constant goblet cell production which can create a consistent vaginal discharge in the healthy state.
An apical cap of sigmoid tissue is an alternative laproscopic surgical procedure to create or lengthen a neovagina. The penile skin available is used for labia minora and ventral penile flaps form the meatus of the urethra. As colonic tissue is used, this vagina will have constant goblet cell production which can create a consistent vaginal discharge in the healthy state.
Diversion vaginitis produces a malodorous discharge when the sigmoid tissue becomes inflamed due to a nutrient deficiency of short chain fatty acids/ butyric acid required for enterocyte health. This can be treated with sodium butyrate or mesaline foam locally.
 This microbiome is more similar to the colon with higher levels of lactobacilli than purely epidermal tissue. Therefore, boric acid capsules and/or lactobacillus probiotic capsules may be prescribed for stubborn discharge or irritation. The sensitive mucosa may not respond well to frequent soap and water rinses; pure water or lightly acidified rinses with 1/2 tsp vinegar or additional lactobacilli may be better tolerated.
This microbiome is more similar to the colon with higher levels of lactobacilli than purely epidermal tissue. Therefore, boric acid capsules and/or lactobacillus probiotic capsules may be prescribed for stubborn discharge or irritation. The sensitive mucosa may not respond well to frequent soap and water rinses; pure water or lightly acidified rinses with 1/2 tsp vinegar or additional lactobacilli may be better tolerated.
DDX: Discharge or bleeding in sigmoid derived neovagina
- Diversion vaginitis
- Inflammatory bowel disease
- Malignancy
- STI – mucosal tissue is more succeptible than epidermal tissue
- Arteriovenous malformations
- Vasculitis
- Diverticulum
Cancer screening:
There are 4 published cases of transfeminine neovaginal squamous cell carcinoma. These may present decades after initial reconstruction surgery. Vaginal discharge was the presenting symptoms in all cases. Bleeding and pain were also present. Any patient presenting with bleeding should under vaginal speculum examination followed by swab and biopsy of any suspicious lesions.
Tumor masses are primarily located at the posterior wall or apex, making self-identification difficult. Sigmoid neovaginas are more likely to present with adenocarcinoma due to embryonic germinal lines.
Annual follow up for transgender women with speculum and digital examination is recommended for cancer screening, assessment of depth and girth,and exclusion of granulation tissue. Speculum exams are generally well tolerated. In one study 84% of transfeminine women would appreciate this follow up examination. Only 4% of the study had ever had a gynecological exam after vaginoplasty. An anoscope can also be used vaginally as a speculum alternative.
Urethral complications
Post surgical lower urinary problems are not uncommon: spraying and upward stream were the most common presentations. Urethral stenosis may require meatomy. Urethral strictures are also possible: rule out post bulbar strictures as well as meatal stenosis as most transwomen will still have a prostate. Urethrovaginal fistulas may also occur: “the majority of cases do not need or require immediate intervention and in most cases the pt will still be continent.” – Dy, Geolani et al. However, bladder-vaginal fistulas require surgical intervention from a transgender urologist.
UTI prevention is the same for cis and transwomen: urinary and sexual hygiene including urinating after sex, wiping front to back, avoiding vaginal penetration after anal penetration, wearing cotton undergarments and using essential oil scented or unscented soaps and body washes on the genitals. Urinary acidification measures may also be preventative – daily cranberry pills or unsweetened cranberry juice, vitamin C and/or D-mannose powder for those prine to chronic high bacterial loads.
Works Cited
- Cornelisse, Vincent J., et al. “The medical care of the neovagina of transgender women: a review.” Sexual Health, vol. 14, no. 5, 2017, p. 442.
- Dy, Geolani W., et al. “Reconstructive Management Pearls for the Transgender Patient.” Current Urology Reports, vol. 19, no. 6, 2018.
- Fierz, Ronja, et al. “Squamous Carcinoma of the Neovagina after Male-to-Female Reconstruction Surgery: A Case Report and Review of the Literature.” Case Reports in Obstetrics and Gynecology, vol. 2019, 2019, pp. 1-7.
- Meltzer, Toby. “Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People: Vaginoplasty Procedures, Complications and Aftercare.” The Center of Excellence for Transgender Health, transhealth.ucsf.edu/trans?page=guidelines-vaginoplasty. Accessed 13 Mar. 2019.
- Mundluru, S.N., and A.R. Larson. “Medical dermatologic conditions in transgender women.” International Journal of Women’s Dermatology, vol. 4, no. 4, 2018, pp. 212-215.
- Radix, Asa. “Transgender Primary Care.” WPATH Biannual Conference, 5 Nov. 2018, Buenos Aires, Argentina. Lecture.

