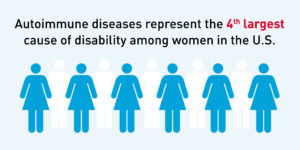
I just finished my final elective of medical school. I chose Rheumatology because I have such a strong genetic tendency towards this class of diseases, and because it was something I felt under-educated about heading into Internal Medicine.
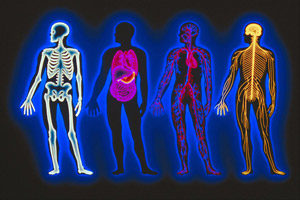
Rheum itself means “a watery fluid that collects in or drips from the nose or eyes.” Whereas rheumatism is “any disease marked by inflammation and pain in the joints, muscles, or fibrous tissue, especially rheumatoid arthritis” according to online dictionaries. Clearly these two do not match up? Although perhaps one could argue it is the “watery fluid” of the joints that is attacked by immune system dysregulation in most of these conditions, resulting in pain, inflammation and joint destruction. 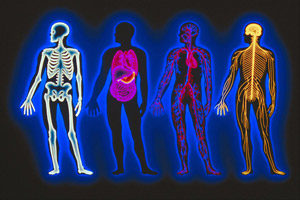 Most of these conditions are also multisystemic, affecting the heart, lungs, kidneys, eyes, skin and more. The umbrella of rheumatology is large: conditions I saw in clinic included rheumatoid arthritis, lupus, scleroderma, psoriatic arthritis, polymyositis and dermatomyositis, pseudogout, gout, and polymyalgia rheumatica. There are of course more that I did not witness.
Most of these conditions are also multisystemic, affecting the heart, lungs, kidneys, eyes, skin and more. The umbrella of rheumatology is large: conditions I saw in clinic included rheumatoid arthritis, lupus, scleroderma, psoriatic arthritis, polymyositis and dermatomyositis, pseudogout, gout, and polymyalgia rheumatica. There are of course more that I did not witness.
A large part of patient management involves managing and regulating pain. Opioids are now recognized as crutches inhibiting recovery for many people with long term pain rather than panaceas. Dr Clauw, a pain specialist from Michigan explains this way better than I could, and also addresses several prescription and over the counter medications as well as lifestyle management techniques for living your best life with chronic pain. Watch this YouTube video now, or listen to it while you drive: https://youtu.be/B0EhNajqkdU
One conversation that came up several times was the use of topicals for pain. Many folks cannot take ibuprofen for pain due to stomach or kidney disease, or are already on long term therapy with prescription strength NSAIDS and still have pain.  Voltarin, a topical NSAID was prescribed regularly, specifically for osteoarthritic pain at the base of the thumb with good success.
Voltarin, a topical NSAID was prescribed regularly, specifically for osteoarthritic pain at the base of the thumb with good success.
Many patients use CBD preparations for consistent pain reduction. Some people call cannabiboids “opioid sparing medications” as people can reduce the amount of narcotics needed on a daily basis with the concurrent use of CBD products. The doctors I was working with did not specifically endorse nor did they advise against medical marijuana as Maine is a state where purchase and possession is legal with certification. However, they did support individuals trying topical marijuana preparations of their own initiative for pain management.
The biochemistry of cannabinoids is super interesting if you are into psychoneuroimmunology. This recent article from Naturopathic Doctor News and Review does a pretty good job of outlining the basics of CBD oil as well as some of its politics in reference to mental health. Its use in pain management is multifactoral. There are two main cannabinoid receptors in the human body both of which are relevant to rheumatology and management of chronic inflammatory, neuropathic and mechanical pain. CB1 receptors are found throughout the brain and body and are responsible for most of the psychotropic effects; they are also found on osteocytes (bone) and chondrocytes (cartilage). CB2 receptors are primarily on immune cells as well as osteo and chondrocytes. The underlying physiology is complex and still being researched extensively but one thing is clear: cannabis-based medications are effecting in reducing chronic pain via their effect on the the endocannabinoid system in humans and altering pain chemical signalling.

As aggressive autoimmune diseases, most of these conditions require sophisticated, high end medications to manage their progression. I saw many cases of men and women who had life changing benefits from DMARDS, or Disease Modifying AntiRheumatic Drugs. My main take home point from this rotation was if one of my patient is newly diagnosed with one of these conditions, REFER! to a rheumatologist as the medications are advanced and specific. My great-grandmother was bed-bound by 40yo with rheumatoid arthritis and she did not have the benefits of science to treat her disease progression. Even tho I am also a Naturopathic Doctor, I have respect for the powerful efficacy of these medications and do believe they improve and maintain quality of life in potentially destructive conditions like these.
On the other hand, medications alone are often not enough to manage and maintain the best health possible. The 2017 textbook I was given for the elective had a small section at the back for complementary and alternative therapies that have good evidence for rheumatology.
- Vitamin C is an essential component of cartilage and collagen. Supplementation reduced progression of joint and cartilage destruction over time. My Note: Vitamin C is naturally occurring in high levels in many raw fruits and vegetables. This is a great reason to eat fresh raw foods as part of your every day diet with any kind of inflammation or joint disease.
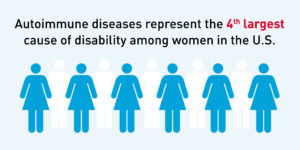
- Vitamin D is for more than strong bones; it is also a hormone that effects immune health. Countries that have less sunlight year round have higher occurrences of autoimmune disease. Get outside 20 minutes daily minimum all year round, and supplement vitamin D every winter. Have your blood levels tested every fall to ensure optimal levels of this hormone and nutrient.
 Fish Oil has known anti-inflammatory properties in its EPA component and many brain benefits in its DHA. This rich omega 3 essential fat is best eaten as a meal at least 3 times per week – a tin of sardines, mackerel or herring has way more nutritional value than a couple of fish oil pills and costs so much less. Any seafood will contain fish oil – the littler the fish, the higher the benefit when it comes to these healthy oils. If you do go for the fish oil pills know that you get what you pay for. Evidence shows you need about 3000mg of fish oil via pills daily for benefit, or at least 450 mg DHA and 750mg EPA. I like Nordic Naturals Brand for best quality and efficacy if you are going to go the pill route. For tinned fish, there are lots of brands, but this is my fave and it’s easy to find in regular grocery stores.
Fish Oil has known anti-inflammatory properties in its EPA component and many brain benefits in its DHA. This rich omega 3 essential fat is best eaten as a meal at least 3 times per week – a tin of sardines, mackerel or herring has way more nutritional value than a couple of fish oil pills and costs so much less. Any seafood will contain fish oil – the littler the fish, the higher the benefit when it comes to these healthy oils. If you do go for the fish oil pills know that you get what you pay for. Evidence shows you need about 3000mg of fish oil via pills daily for benefit, or at least 450 mg DHA and 750mg EPA. I like Nordic Naturals Brand for best quality and efficacy if you are going to go the pill route. For tinned fish, there are lots of brands, but this is my fave and it’s easy to find in regular grocery stores.- Omega 3 oil is also available in vegetarian form as flax seed oil or marine algae oils.
The evidence for a specific kind of diet for autoimmune disease is variable. Dr Jackson referenced the Mediterranean Diet as the best foundational nutritional plan for Lupus specifically. This makes sense as it is a low inflammatory, high fruit, fiber and vegetable diet with known benefits for heart health and longevity.
Many people choose to go paleo, or follow the whole 30 autoimmune diet plan. Phoenix Helix is a podcast dedicated to autoimmune health and paleo nutrition. During my rotation I listened to a great episode with Dr. Aly Cohen, an integrative rheumatologist who spoke on scleroderma and integrative medical management. In addition to reviewing some specific suggestions for scleroderma, Dr. Cohen spoke on the importance of reducing processed food chemicals, pesticides and additives and choosing clean drinking water, not from plastic bottles. As she said, over 90,000 chemicals have been introduced to the ecosystem and therefore the human body in less than 100 years. Autoimmune disease is linked to this toxic burden and inability to process the chemicals. Find out more about her work @thesmarthuman on Twitter and Facebook.
 Three weeks of rheumatology clinic was only enough to learn the basics of diagnosis and management, and gave me great respect for my fellow Rheumatologicial internists. Each of the conditions under the Rheumatology umbrella have advanced immune dysregulation and multisystemic consequences with potentially dire outcomes. Fortunately, pharmacology has a class of exceptional medications that work quite well, especially when paired with nutritional initiatives and long term pain management strategies that focus on quality of life. I am grateful to Dr. Stanhope and Dr. Jackson at Central Maine Medical Center Rheumatology Associates for letting me ask too many questions while they were trying to write notes during their busy clinic days – and for the freedom to enjoy afternoon sunshine on my last medical school rotation!
Three weeks of rheumatology clinic was only enough to learn the basics of diagnosis and management, and gave me great respect for my fellow Rheumatologicial internists. Each of the conditions under the Rheumatology umbrella have advanced immune dysregulation and multisystemic consequences with potentially dire outcomes. Fortunately, pharmacology has a class of exceptional medications that work quite well, especially when paired with nutritional initiatives and long term pain management strategies that focus on quality of life. I am grateful to Dr. Stanhope and Dr. Jackson at Central Maine Medical Center Rheumatology Associates for letting me ask too many questions while they were trying to write notes during their busy clinic days – and for the freedom to enjoy afternoon sunshine on my last medical school rotation!