My IG and twitter feeds keep sending me promoted ads for intermittent fasting and young thin women in my Internal Medicine residency program keep telling me they are doing it. As someone with an inherent red flag signal for anorexia and eating disorders, I am triggered. As someone with a 4 year nutrition degree and as a gal raised with a spiritual practice of fasting, I do understand the value behind the concept. The problems start when restriction/binging/restriction patterns are overlayed on the foundational evidence.
This is the best nutritional protocol and evidence I found to implement intermittent fasting into a food plan for weight loss or for longevity. There is good reasoning and practice behind the idea that the liver stores glycogen for storage, and that this “immediate use” supply needs to be used up before the body creates new glucose from adipose cells and muscle. This is reasonable: fasting uses up the supplies . Then fasting decreases fat or muscle from stores.
Some fasting articles I’ve read suggest 16 hours between eating every day. This sounds alot like the “don’t eat food after 7” rule that has quite a few generations of folks waking up covered in cookies from night eating.
Some articles suggest 16 hours between meals twice a week. This seems more reasonable to me as it allows for some pre-planning to have restful, quiet time during the fasting period. Our human bodies are not designed to “run on empty.” I grew up in a yoga community where fasting was part of the practice towards enlightenment, but work was not done during the fast. One’s time in the fasting state is to be spent meditating, reflecting, and processing (like while we sleep.) Yoga is also an acceptable practice during this time as it stimulates glands and organs as well as the musculoskeletal body to return to homeostasis. Fasting is designed as a parasympathetic state to rebalance CYP liver enzymes and clear the intestines. Pushing through fasting with sympathetic, highly motivated activity like mental or physical labor requires the adrenal glands to overachieve and drive metabolism through adrenaline and sheer will aka cortisol.
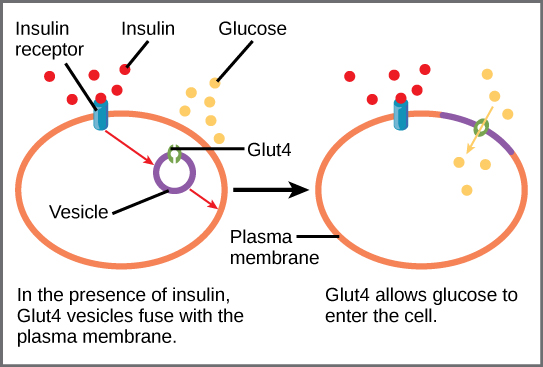
The one place where hard work on a fasting belly IS indicated is for anyone looking to lower insulin resistance by using the biochemistry of exercise. This could be someone requiring huge doses of insulin for only moderate blood glucose control, or someone trying to beat type 2 diabetes in the pre-diabetic state. Exercising on an empty stomach is one of the few ways to upregulate cellular receptors called GLUT_4 for insulin to bring blood sugar into cells. I have tried this and its oddly satisfying. Nerd out on biochemistry and GLUT-4 here.
I don’t intermittent fast intentionally myself. Some weekend days I wont eat food until 2-3 in the afternoon, just based on my natural appetite; however, I do have black coffee and water and sometimes juice during that time. To be my best self, I need frequent and regular fuel to keep this brain and body going for the intense work weeks I do. Not allowing myself to eat when I am hungry in not helpful for my mental health either – not only do I get edgy or feel anxious, my own disordered eating and body dysmorphia can easily be motivated towards restrictive eating patterns.
Aside from mental health, some people also have genetic metabolic imbalances if their lineage experienced a traumatic food restriction. This has been researched in Irish descendants as well as Jewish folks. Caloric restriction can actually trigger a survival metabolism where minimal resources are burned and every morsel of fat possible is stored. This is ancestral trauma that has caused permanent alterations in the genome that get triggered by environmental circumstances.
The science is compelling: improved metabolism, destruction of cancer cells, immune regulation, cortisol balancing, cellular rejuvenation…. benefits are numerous!
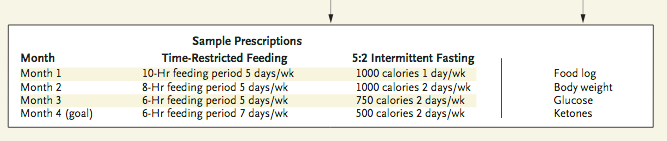
Here is what I would do if I was either doing a period of cleansing/detox and intentionally working on restoring health or if I was committed to a defined period of intentional weight loss (8 months from this algorithm.)
- Style 1: two mornings a week, fast until 12-1pm depending on your 16 hour window. On these mornings drink warm water, organic green tea or herbal tea, stretch and do yoga or go for a gentle walk, get into nature, rest/ meditate, write or reflect. Eat a Mediterranean style diet the remainder of the time.
- Style 2: For a more intensive weight loss experience, follow the algorithm for 2 days a week of restricted caloric intake from the JAMA article referenced at the beginning of this post. I would not also follow the time restricted feeding patterns myself as I find this too rigid for modern life and overrides the natural appetite instincts which are essential. Eat a Mediterranean type diet or Paleo. Consider pairing this with the Whole 30 protocol or an elimination diet for true restorative food as medicine. Follow the above guidelines for your calorie restricted days with rest, nature, reflection, massage, acupuncture or other healing practices, whole organic foods, teas and water. Once you have completed month 4, return back up the protocol until you are back at full weekly caloric intake and reassess.