Half an inch from the first four thoracic vertebrae lie the central nervous system transistors (stellate ganglion) for your fight and flight nervous system. Needless to say, my upper back is constantly aching. I am metabolizing the unique stress of being a brand new doctor/medical student in hospital life. It’s a different kind of stress than the first two academic years: those were crushing content & exams, but they were ivory tower academia. This is the very real medicine that is literally birth, life and death stuff. More visceral than literal, I find myself often crying, sometimes gagging, and occasionally elated.
Half an inch from the first four thoracic vertebrae lie the central nervous system transistors (stellate ganglion) for your fight and flight nervous system. Needless to say, my upper back is constantly aching. I am metabolizing the unique stress of being a brand new doctor/medical student in hospital life. It’s a different kind of stress than the first two academic years: those were crushing content & exams, but they were ivory tower academia. This is the very real medicine that is literally birth, life and death stuff. More visceral than literal, I find myself often crying, sometimes gagging, and occasionally elated.
The purpose of third year clerkship aka #MS3 is to get a sampling of each major specialty to help us decide on a residency. Its a generic med school formula consisting of: Pediatrics, Surgery, OB/GYN, Internal Medicine Inpatient & Outpatient, Family Medicine, Psychiatry, Community Health. Inpatient, we legally cannot write patient notes. While we can actively participate in patient care, everything we do needs to be seconded by a licensed doc; therefore, we are mostly shadows, errand runners, and absorbent sponges.
Unfortunately, some throwbacks to fraternal physician hazing rituals are still in place even for third year medical students. For example, my Internal Medicine inpatient rotation, which is already a 6am – 6pm shift 5 days a week (with a 1 hr drive on each side) also requires 6 -24 hour shifts in the 6 weeks. I asked a friend who is a year ahead of me and attended a different hospital clerkship if her rotation was scheduled as such, and she said she had to follow hospitalist hours for that same rotation – roughly 730am – 330pm. If the point is to learn each of the specialty’s roles, it makes sense to follow the professional hours. If the goal is to teach us that Internal Medicine requires an exhausting slog of hospital life, and how to forsake all other aspects of our personal and academic life for our career, then this approach in third year makes sense. Slate Magazine said it best: Third Year Kills Humanity of Medicine.
I haven’t done the above inpatient IM rotation yet and yes, I’m actively worried about my health, my marriage, and my coping skills during that onslaught. I did one 86 hour “sneak peek” week with our Family Medicine inpatient service last Fall. I did enjoy the steep learning curve and patient contact; however, I often felt lost and useless as my resident dictated her many notes and ran around the hospital following up on pages and other details. I did get some good studying done and learned some basic inpatient skills but there were hours, especially after the first 8, that I wished I had something more productive I could be doing in.
In reality, the residents are much more forgiving than the administration and often let us leave early (6am – 10/11pm) saying “there is nothing we could learn at 2am that cant be learned at 2pm.” I am eternally grateful for this ray of grace. And I do understand that night shifts and on-call hours are foundational for many physician careers and practicing them could be relevant. But why, when 55% of Internal Medicine and Family Doctors report burnout, are we being subjected to these mind numbing hours as third years? How will medicine ever change if the hazing continues to be perpetrated generation after generation?
I accept that being a doctor requires selflessness & sacrifice. I accept that long hours are often required and I like to work – for an income, for a team, and for a good reason. I’m a second career medical student, I study and practice clinical skills because this is what I love! I accept that as a resident I will bear the brunt of hours spent watchdogging and admitting in part because we are the cheap labor force of institutionalized medicine. But, I have 1.5 years of med school left, and 3-6 years of residency/fellowship ahead. What is the purpose of having me work 86 hour weeks now, and how is it going to benefit my relationship towards medicine?
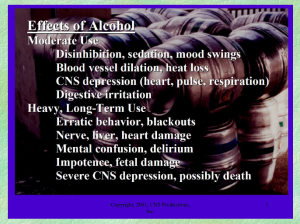
 To embed resilience in doctors, we as a profession and as an academic incubator need to provide time & space for rest, relaxation, and quietude. Only in parasympathetics can we metabolize the soul-rattling experience that comes from facing death and sickness and the burden of chronic disease in North America. Not only are we facing grief/loss/mortality, we are taking on the enormous responsibility of decision maker. A backlog of unprocessed emotion leads to substance abuse, chronic pain, sleep disorders, lack of compassion, and who knows what other organic & chemical dysregulation. We need regular daily time to cook good food, sleep with our loves, be intimate and vulnerable, Netflick and chill, get to the gym or get outside. Only in that space can we emotionally integrate this transformation.
To embed resilience in doctors, we as a profession and as an academic incubator need to provide time & space for rest, relaxation, and quietude. Only in parasympathetics can we metabolize the soul-rattling experience that comes from facing death and sickness and the burden of chronic disease in North America. Not only are we facing grief/loss/mortality, we are taking on the enormous responsibility of decision maker. A backlog of unprocessed emotion leads to substance abuse, chronic pain, sleep disorders, lack of compassion, and who knows what other organic & chemical dysregulation. We need regular daily time to cook good food, sleep with our loves, be intimate and vulnerable, Netflick and chill, get to the gym or get outside. Only in that space can we emotionally integrate this transformation.
Our clerkship Dean Dr. Taylor sent out this reaffirming blogpost last month in which an experienced physician Dr. Youngson writes to his younger self. He says:
“As a medical student or junior doctor, it’s easy to feel powerless especially in a hierarchical medical system that too often teaches by humiliation, punishes those who question the status quo, and grinds people down through overwork and inhuman working conditions…”
Change medical education so that we as medical students (and residents and attendings and all doctors actually) are seen as people who are more than life-saving, problem fixing, chart dictating, disease curing machines. A more gentle, humane practice of time & space for medicine while living life alongside the role of physician has to start at the beginning of the clerkship year when we integrate it’s practice with our academic foundations, or it wont be ingrained as part of the way we approach medicine.
Once I started thinking about time, resilience and integration as the cure of medical burnout, I began seeing evidence everywhere. I heard a NEJM Interview from 01/03/18 with Dr. Armstrong from Massachusettes General Hospital’s new Pathways program where residents are given time and a scientific team to investigate complex patient-based cases. The 12/26/17 issue of JAMA has an article by Jack Coulehan, MD MPH from the Center for Medical Humanities, Compassionate Care and Bioethics on Negative Capability and the Art of Medicine that speaks to “sustaining the physician through the ‘humdrum routine’ of professional life… [Using]… the power to recognize the ‘true poetry of life'” and of medicine. This is a reflective practice. He says:
“In pursuing the steadiness and detachment required to master clinical practice, it is tempting to neglect the more difficult project of nourishing engagement and tenderness in our relationships with patients – and with ourselves.”
The future of medical education is not only about competencies met and clinical acumen. The true scholars of the next generations of physicians will be those who can achieve their best in patient care and scientific fulfillment, while also living a satisfying, integrated and joyful life.