Some people fall asleep fine but cannot stay asleep. Like other sleep pathology this can be due to a complex interplay of underlying reasons. Often the 24H cortisol circadium rhythm has become dysregulated and the early morning peak is coming earlier than it should, waking people up at 3, 4 or 5am. What can be done? There are some prescription sleep medications that can be helpful, and global stress management skill building is also important. Underlying anxiety disorder may need to be treated and substance use disorders are also major players in sleep-wake disorders.
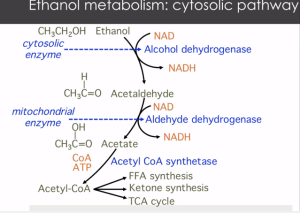
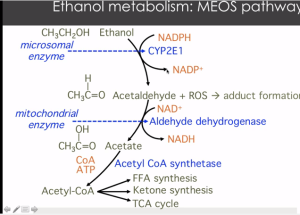
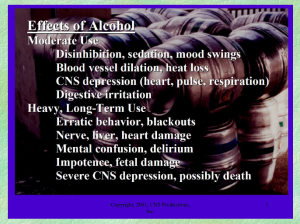
Alcohol is an obvious player in the 3am waking game. For people who drink regularly, depending on what time one goes to bed and therefore stops drinking, at some point the alcohol with start to wear off and the withdrawal will start bringing agitation, heart palpitations, sweating, and headache. This can cause early morning waking between 3-5am. Chinese medicine correlates each organ to a 24H clock, and this time of day is the Liver time. Ironic, yes? Accurate, yes? Decreasing evening alcohol can certainly result in better sleep. Alcohol free evenings may take some time to produce better sleep but after about 7 days of abstinence the sleep cycle will begin to regulate. If full abstinence is not desired, start by at least assessing the effect of alcohol and considering your own motivations for changing drinking patterns as they do certainly effect sleep negatively. Having some protein closer to bed time can be stabilizing to blood sugar and alcohol metabolism overnight.
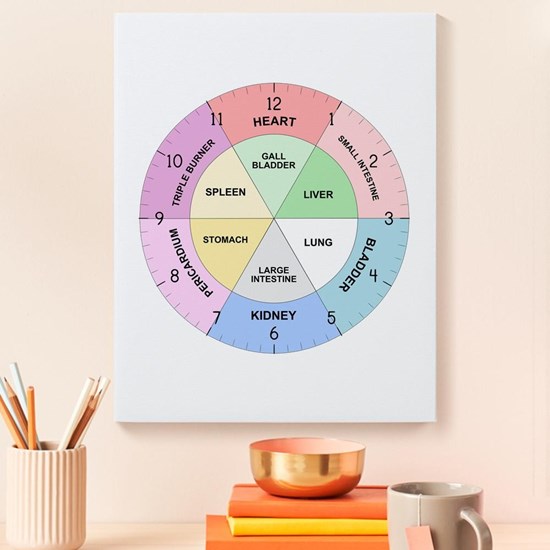
This is true for diabetics as well as for people using alcohol. This is not my area of expertise, but diabetes is related to increased cortisol levels due to the connection between fasting blood glucose, blood sugar, and the liver and pancreas control of blood sugar during the overnight fasting period. There are several studies on sleep disorders in people with diabetes which have evidenced that there are clinical correlations. If you have diabetes and poor sleep, I recommend working with your PCP or Diabetes specialist to make sure your blood sugar issues are not the root cause before moving into more behavioral or psychiatric sleep medications and sleep medicine studies.
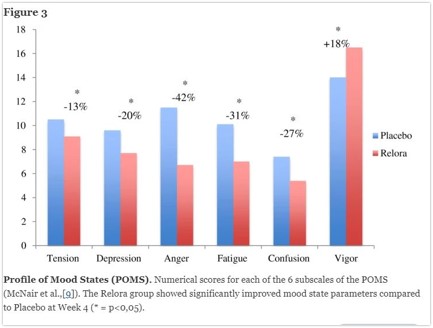
The first botanical medicine I turn to when faced with early waking is a version of several different formulations using standardized botanical extracts of magnolia. The first agent that was trademarked was called Relora and was a Canadian product. This standardized extract regulates disorderde circadiuan rhythms. Whan taken at night it helps smooth out early morning cortisol spikes, decreasing early morning waking related to stress and anxiety. It also has some evidence to decrease stress related eating, and improve subjective mood and wellbeing.
A similar American product is Cortisol Manager by Integrative Therapeutics. This product also uses the honokiol standardized extract with magnalol rather than berberine. This product is combined with ashwaganda (Withania somniferol). Ashwaganda also has evidence that it adjusts dysregulated cortisol circadian rhythms for improved early morning waking. There are many sleep formulations available that contain Ashwaganda. Gaia brand “Sleep Thru” formulation is another similar product for use when early waking is the issue rather than difficulty falling asleep.
These botanical formulas are generally safe for people without significant health conditions. If you are taking more than 5 medications, have kidney disease CKL3 or greater, or are on immunosuppressive drugs for transplants, autoimmune disease or any other indication, supplements should not be taken randomly without supervision by a licensed Naturopathic doctor or trained herbalist as there could be real drug-herb interactions.
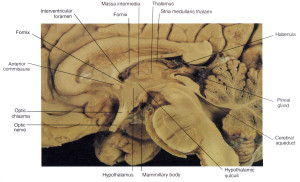
Finally, as mentioned at the beginning, emotional stimuli do go thru hypothalamic-pituitary-adrenal axis to effect cortisol secretion. Lifestyle modifications are necessary in every case to at least consider the underlying causes of the stress. A pill alone cannot regulate a deeply engrained habit or pattern. Most health care providers would like to hear about what is keeping you up at night, in order to troubleshoot with you ways to improve coping and reduce suffering. These plant based medicines are allies in your journey towards improved health and are only part of the team based approach that real change towards health entails.
lDeshpande A, Irani N, Balkrishnan R, Benny IR. A randomized, double-blind, placebo-controlled study to evaluate the effects of ashwagandha (Withania somnifera) extract on sleep quality in healthy adults. Sleep Med. August 2020;72:28-36.
Talbott, S.M., Talbott, J.A. & Pugh, M. Effect of Magnolia officinalis and Phellodendron amurense (Relora®) on cortisol and psychological mood state in moderately stressed subjects. J Int Soc Sports Nutr 10, 37 (2013). https://doi.org/10.1186/1550-2783-10-37