I am giving a webinar this week to a group of cardiologists on all gender cardiology. Spoiler alert, there is no difference between cis and trans gender heart health. The differences lay in access to health care, stereotypes about hormone therapy, and minority stress. For cardiology, once you have a sick heart, regular physician follow up is crucial to your care – multiple medications are sometimes needed to improve or preserve heart function and imaging is needed over a lifetime to track structure and function. If a person does not feel safe at their cardiologist’s office because they are constantly called the wrong name or experience microaggressions about their body, that person will avoid going back or drop out of care all together. Therefore, the first and most important point of all gender cardiology is creating a safe medical home with dedicated staff and physician training in transgender and gender diverse specific health care.
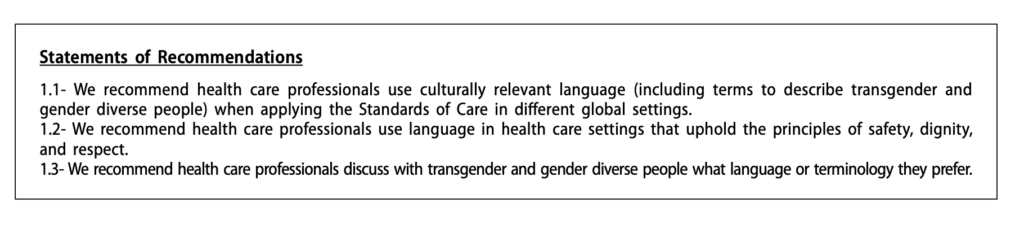
Documentation matters. Medical charts are living documents of a patients experience and how we represent someone matters both for the patient and for all the people who read the document. Safety, Dignity and Respect are basic human rights which are not always upheld for gender diverse individuals, even in a doctors office. Do not be afraid to ask an individual what terms, names, pronouns they would like used in their chart. Asking is consent and consent is powerful. Some terms have fallen out of favor over the last 2 decades that I frequently hear used in the hospital such as Male-to-Female (MTF) and Female-to-Male (FTM). These have been replaced with assigned gender at birth attached to current gender presentation, or just gender presentation. Assigned gender at birth includes Assigned Female at Birth (AFAB) and Assigned Male at Birth (AMAB.) These can be helpful in a medical setting bc they may signify reproductive organs present ( or they may not depending on surgical interventions.) Some gender diverse folks feel passionately against AMAB/AFAB as well because they focus more on the assigned birth gender than the current gender. Therefore, in documentation, either ask the patient how they would like to be represented, or consider using a hybrid like AMAB transwoman, or just transwoman in your notes.
Cardiology and IM are frequently consulted for assessment prior to surgery. Treat gender diverse folks the same as you would anyone else. For a long time gender affirming hormones were stopped prior to surgery, especially estrogen for transfeminine patients due to the heightened risk of venous thromboembolism. This practice is no longer recommended. We would not put a cisgender person on hormone blocking agents for a surgery; therefore, stopping all hormone treatment for transgender individuals does not make sense. In fact, continuation of hormone treatment is beneficial for withdrawal prevention, mental health and for prevention of side effects of hypogonadism including osteoporosis. Continue the current therapy through surgery and risk stratify/ treat perioperatively as you would any other patient with RCRI, MINS screening and DVT prophylaxis.
For more on gender and plastic surgery see this collection of 11 special topics on gender surgery from the Journal of the American Society of Plastic surgeons.
“Hontscharuk and Schecter assemble the most
comprehensive review of literature from plastic sur-
gery, gynecology, and endocrinology to consider the
risk profile of transgender hormones and surgical
venous thromboembolism. One surprise of their
well-sourced study is that the risk of perioperative
estradiol may be lower than commonly thought.
High rates in early series are attributed to the use
of oral ethinyl estradiol and high doses, with newer
regimens showing lower rates. One area where the
literature is limited, however, is in quantifying cur-
rent practices in hormone cessation. In a survey of
six high-volume vaginaplasty centers (unpublished
data), all surgeons still stopped estradiol 2 to 4 weeks
before surgery.”
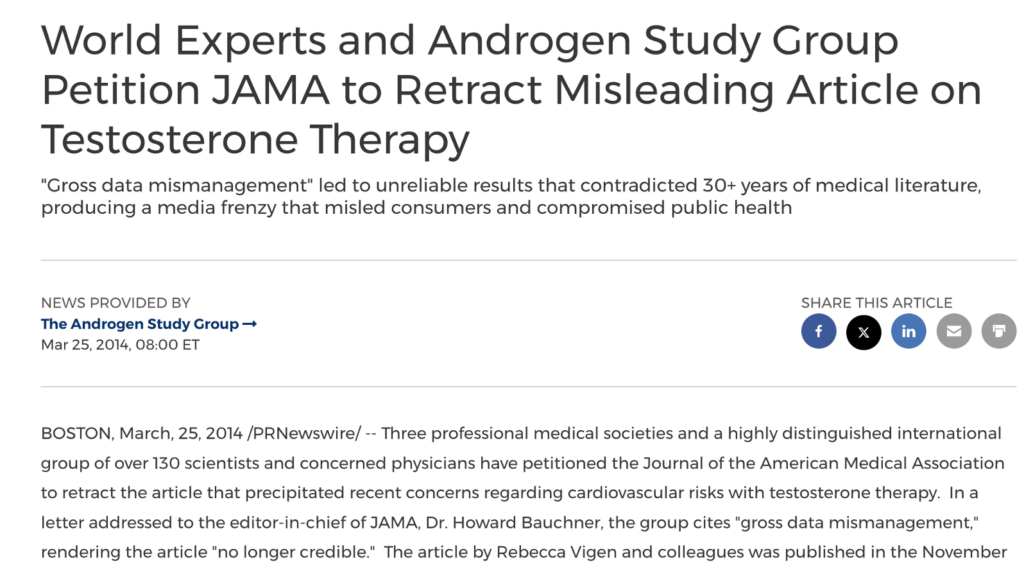
Ok, now we can finally start talking about the heart and gender affirming hormones, starting with testosterone. This topic applies to anyone who has testosterone including cisgender men but is specifically for transmen and nonbinary people using testosterone. As the rise of ‘andropause” or mens antiaging medicine came into the public eye, the medical assumption was that because men had more cardiovascular disease (CVD) and men had testosterone, therefore testosterone increased heart disease risk. This was pure conjecture and has not held up in any evidence based investigations. A 2014 JAMA article was published from VA data-mining that stated that hypogonadal men starting testosterone had increased risk of MI, with the declaration that therefore testosterone was not indicated in anyone with increased cardiac risk or cardiac disease. The article was quickly retracted and amended as the data was corrupted (multiple patients with MI’s had not started the testosterone, ciswomen not on testosterone were included in the MI population.) The damage was done, and many people still believe the false claims a decade later.
Testosterone therapy is vital for gender diverse patients who need masculinization. Even if it did carry a CVD risk, the beneficial effect of mental and physical wellness for gender congruence would be worth the possible risk. Because of its importance in transgender medicine, this is an ongoing hot topic of research to better understand the nuances and possible risks of testosterone therapy.
“A large 2018 case control study from several US centers that used 10:1 cisgender matched controls found no statistically significant difference in rates of MI or stroke between transgender women and cisgender men, a rates of MI, stroke, or venous thromboembolism (VTE) between transgender men and cisgender men or women. There was a statistically significant hazard ratio of 1.9 for VTE among transgender women when compared with cisgender men.” CH 15 WPATH SOC
The relationship between testosterone and trans health is important enough that the American Heart Association investigated and released a scientific statement in 2021, because trans and gender diverse folks of all genders HAVE consistently had worse cardiovascular morbidity and mortality than age matched peers.

However, in the anti-aging and cisgender mens health community the question of cardiac safety with testosterone hormone replacement lingered. In 2015 after the original data debacle, the FDA required companies making approved testosterone products to participate in clinical trials to elucidate the evidence. The Testosterone Replacement Therapy for Assessment of Longterm Vascular Events and Efficacy Response in Hypogonadal Men (TRAVERSE) trial was created and just published in 2023.

Testosterone HAS been repeatedly shown to decrease HDL, the protective scavenging cholesterol and increase triglycerides. It evidences variable effects on total cholesterol and LDL . This could be a piece of the puzzle for increased CVD risk in trans men, but has not been definitively proven yet. Regardless, exercise is the best way to increase HDL in all genders, so as health care providers we need to continue motivational interviewing for active lifestyles, 150minutes of exercise weekly and lipid-conscious nutrition for all our patients including trans men.
So why are transmen more likely to have cardiovascular disease? The the answer is multifactoral and boils down to lifestyle and and health care access which crosses many intersections of class, and race, minority stress and more (which is another important conversation). Heart disease is a cumulative pathology. Unless one has a congenital heart condition, it takes decades of uncontrolled alcohol use, dysregulated blood sugar, nicotine toxicity, low nutrient and high fat foods and sedentary lifestyle to generate atherosclerotic coronary disease. Prevention is the best medicine for a healthy heart and vasculature, but prevention also means having a doctor to work with for things like blood work and blood pressure measurement. If you are someone who has a bad experience in the medical world, or worse, someone who is denied care due to your gender or sexuality, that person will often have worse outcomes with age.
TBC in the next post – ESTRADIOL! – because this one is getting long!