The Mediterranean Diet (and Lifestyle)
The Mediterranean Diet (and Lifestyle)
This post was originally written for Apothecary by Design.
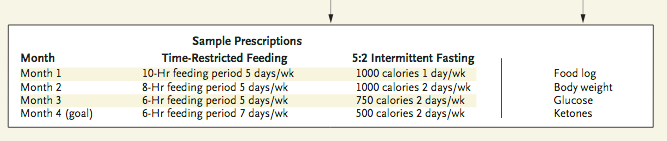
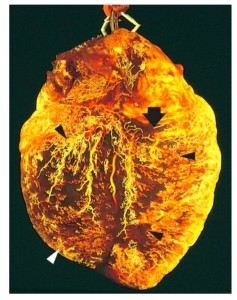
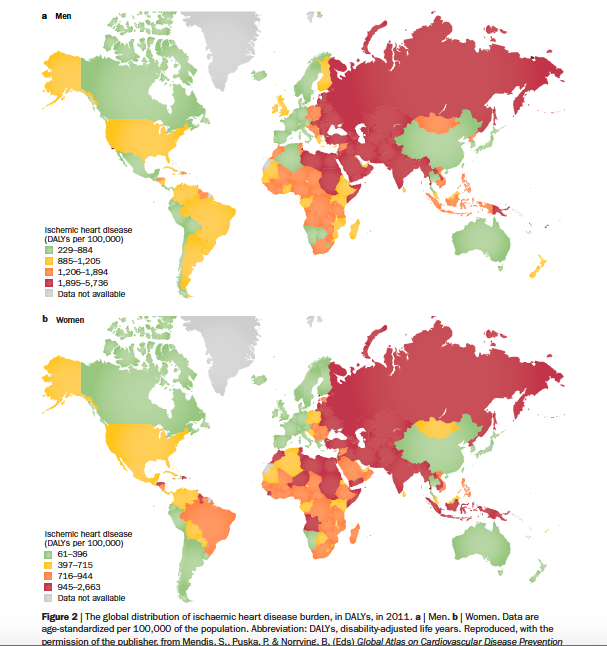
There is a lot of conflicting opinions about what style of diet individuals should choose for best health. Eating patterns can be based on ethics, habits, familial patterns, disease states, weight loss, convenience and more. The Mediterranean Diet is specifically known to correct heart disease, high blood pressure and high cholesterol. It is also used in cancer recovery. It is not a prescribed regimen of foods, but rather a way of eating based on the local foods of indigenous cultures that live around the Mediterranean Sea. People from this region tend to live longer, and have less chronic disease and obesity than the rest of Europe and North America. To understand why, scientists looked at the foods and lifestyle of the region which has been proven time and time again as superior for cardiovascular health and wellness.
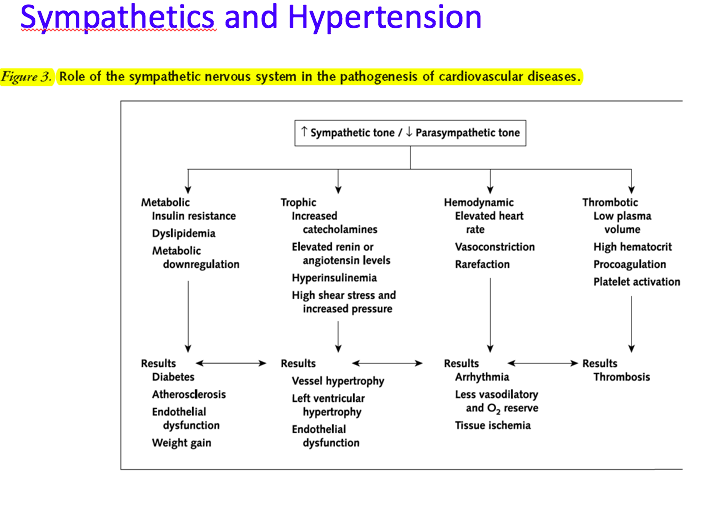
Introduction: It is estimated that over 600 million people have high blood pressure. Heart disease is still one of the leading causes of death in the United States, and dietary interventions are first line therapies for prevention and treatment. The Mediterranean Diet, so called because it mimics classic eating patterns and ingredients from countries like Spain, Italy and Greece, has proven itself time and again as an effective therapy for hypertension and cardiovascular disease. A quick search of Medscape will show you that other conditions like Type 2 Diabetes, Weight loss, Alzheimer’s disease, Metabolic Syndrome, and Cancer are also being improved by adherence to this style of eating.
What it entails: The Mediterranean Diet is modeled after a traditional European “local” diet. Think small servings of homemade pasta or polenta, with fresh local herbs and vegetables like rosemary, basil, tomato, fennel, mushrooms and onions sautéed in liberal amounts of extra virgin olive oil. Add some white beans or fresh local cheese and handfuls of fresh arugula. Small fish like sardines and anchovies are added to meals regularly or served as a snack with walnuts, flatbread and cut up raw vegetables like cucumbers, cabbage, carrots, and broccoli. Fish is a regular staple, always cooked with olive oil and often marinated with lemon and fresh herbs. A couple times a week you may have free range eggs or chicken, again with liberal amounts of greens, cooked vegetables, beans and fresh herbs. And steak or lamb is eaten a couple times a month. Red wine is served with dinner most nights, and small amounts of homemade dessert like tiramisu or gelato a couple times a month.
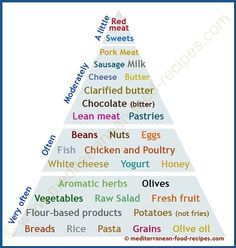
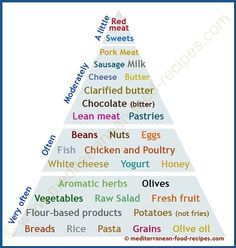 Many people use a triangle to depict the major Food groups for the Mediterranean diet.
Many people use a triangle to depict the major Food groups for the Mediterranean diet.
Grains and pastas while frowned on by the low-carb crowd, are important for feeling full, serotonin production, daily fiber and vitamins and minerals. They are also essential for T3 thyroid hormone production. Grains are commonly used in their whole form for optimal nutrition although some homemade pasta and bread are implemented. Suggested Mediterranean grains include barley, buckwheat, bulgur, cous cous, farro, millet, polenta, rice, and wheat berries. Whole grain salads and porridges are great ways to have a daily grain in your menu. Portion sizes are conservative, with emphasis on the vegetable and olive oil.
Vegetables are an important staple in the eating patterns of all countries bordering on the Mediterranean, providing essential plant nutrients, vitamins, minerals and fiber. Cook with virgin olive oil, and drizzle whole pressed plant oils on raw vegetables. These plant nutrients and plant oils are thought to be the foundation of the beneficial effect from this way of eating as they provide essential fats and omegas daily. Commonly used vegetables include: artichokes, arugula, beets, broccoli, Brussel sprouts, cabbage, carrots, celery, celeriac, cucumber, dandelion greens, eggplant, fennel, greens of all kinds including collard, kale, Swiss chard and more, leeks, lemons, lettuce, mache, mushrooms, okra, onions, peas, peppers, potato, pumpkin, radish, rutabaga, scallion, spinach, turnips, yams and zucchini.
Whole fresh fruit provides sweetness and important nutrients, with juicy sweetness. Include apples, apricots, avocado, cherries, clementines, dates, figs, grapefruit, pomegranate, strawberries and tomatoes. Avoid juices, jams, and jellies as these are high in sugar without the antioxidants and fiber of whole fruit.
 Nuts and Seeds are another key to the healthful oils that improve cardiovascular health. One study added only walnuts to a standard diet and exhibited cardiac disease improvement just from the omega 3 fats naturally contained in these nuts. Twenty raw almonds daily have also been suggested as a natural way to lower blood pressure. All raw nuts and seeds and raw nut butters except peanuts contain beneficial oils and add richness and flavor to vegetable based dishes. Once you “dry roast” or roast the nuts and seeds, the beneficial oils are lost or made into inflammatory trans-fats. If you prefer the taste, buy raw nuts and toast them yourself in a cast iron pan or a low heat oven for 10-20 minutes. You can add spices, soy sauce or honey before toasting for additional delicious taste!
Nuts and Seeds are another key to the healthful oils that improve cardiovascular health. One study added only walnuts to a standard diet and exhibited cardiac disease improvement just from the omega 3 fats naturally contained in these nuts. Twenty raw almonds daily have also been suggested as a natural way to lower blood pressure. All raw nuts and seeds and raw nut butters except peanuts contain beneficial oils and add richness and flavor to vegetable based dishes. Once you “dry roast” or roast the nuts and seeds, the beneficial oils are lost or made into inflammatory trans-fats. If you prefer the taste, buy raw nuts and toast them yourself in a cast iron pan or a low heat oven for 10-20 minutes. You can add spices, soy sauce or honey before toasting for additional delicious taste!
Beans and Legumes are great source of protein and fiber and have a rich creamy texture. Cook with cannellini beans, chickpeas, fava beans, and green beans. Kidney beans, lentils, and split peas are also common ingredients in Mediterranean meals. Legumes provide a protein rich flavor note and nutritional support; in moderate amounts they are less likely to cause digestive upset. Think: brothy bowls of rich soup, light summer salads with olive oil and beans, or a Spanish fabada with pork and sausage. Use a digestive enzyme if needed to improve digestion and reduce side effects.
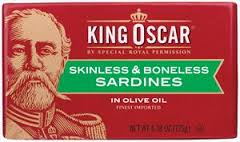
 Fish and seafood are prominent in the way of eating as it is based around sea cultures. Fish and shellfish are incorporated almost daily, providing high amounts of omega three fats essential for heart health. Little fishes like sardines, anchovies and mackerels are cheap and abundant and very high in omega 3 oils. Next time you are at a grocery store, pick up a tin of boneless, skinless sardines. Try eating them with crackers and sour cream, or top a nicoise-style salad with them (potatoes, olives and arugula.) They are quite delicious! Bigger fish like tuna, salmon and sea bass are featured regularly, as well as all shellfish, octopus and eel varieties. Fish and seafood are rarely battered and friend. They are often grilled, baked, steamed or pan-fried with olive oil.
Fish and seafood are prominent in the way of eating as it is based around sea cultures. Fish and shellfish are incorporated almost daily, providing high amounts of omega three fats essential for heart health. Little fishes like sardines, anchovies and mackerels are cheap and abundant and very high in omega 3 oils. Next time you are at a grocery store, pick up a tin of boneless, skinless sardines. Try eating them with crackers and sour cream, or top a nicoise-style salad with them (potatoes, olives and arugula.) They are quite delicious! Bigger fish like tuna, salmon and sea bass are featured regularly, as well as all shellfish, octopus and eel varieties. Fish and seafood are rarely battered and friend. They are often grilled, baked, steamed or pan-fried with olive oil.
Eggs, dairy, meats, wine and sweets are also part of this way of life, but in modest amounts, For example, cheese and yogurt may be eaten daily as tatziki yogurt dip, manchego , romano or feta; you do not see the consumption of large amount of industrialized cheese like a Domino’s pizza. Red meat is enjoyed every couple weeks as are cured meats like salami, carpaccio or prosciutto – used sparingly on homemade pizzas with a cheese like ricotta, or served antipasti with olives and vegetables.
As you can see, there is great diversity in this way of eating. There are no “bad” foods and “good” foods, but there is a plethora of vegetarian and pescatarian eating that results in high vitamin C, E and selenium, high levels of glutathione, balanced omega 6 and 3 oils, high fiber, and abundant antioxidants from fruits and vegetables including resveratrol from red wine and polyphenols from olive oil. These are the basic foundations of a heart healthy diet that any nutritionist or integrative doctor will recommend!
 Longevity Lifestyle: There is more than just food to the Mediterranean success though. Lifestyle is almost equally as important for the longevity and happiness that contributes to this regions wellness. Meals are enjoyed in a social atmosphere, contributing to slower eating and improved digestion. Naps in the form of “siestas” are built into the regions lifestyle, allowing valuable down time and relaxation as well as sleep! Movement, in the form of daily walking and gardening, is an inherent part of an active lifestyle that also improves cardiovascular fitness. And finally, there is a strong sense of community, often centered around religion, which fulfills the esoteric or spiritual needs at an individual level.
Longevity Lifestyle: There is more than just food to the Mediterranean success though. Lifestyle is almost equally as important for the longevity and happiness that contributes to this regions wellness. Meals are enjoyed in a social atmosphere, contributing to slower eating and improved digestion. Naps in the form of “siestas” are built into the regions lifestyle, allowing valuable down time and relaxation as well as sleep! Movement, in the form of daily walking and gardening, is an inherent part of an active lifestyle that also improves cardiovascular fitness. And finally, there is a strong sense of community, often centered around religion, which fulfills the esoteric or spiritual needs at an individual level.
Implementing Changes: The biggest hurdle to changing your nutrition is what you put in your grocery cart. As long as you have frozen meals and industrial cheese in your cupboards, that is what you and your family will eat. Start by purchasing olive oil, fruits, vegetables, raw nuts, and whole grains, and planning simple meals like soups and salads. Scope out your local Italian grocery store like Micucci’s in Portland, and go to the farmers market and fish market for inspiration. Classic Italian, Spanish, Middle Eastern or Greek cookbooks or cooking classes can provide inspiration; however, this is inherently a simple style of eating. Some convenience may be lost as you cook a cannellini bean soup, but the preparation time can be made up by the abundance of delicious, easy leftovers and lunches. Enjoy your preparation time with music and a glass of wine and have your kids help – community and relaxed eating environments are two of the secrets to happiness! Get inspired by these simple recipes.
 A note on olive oil. Americans spend about 700 million dollars on olive oil per year. Low grade olive oil is rampant, and many cheap versions are cut with soybean oil or other inferior vegetable oils. Products branded as Extra Virgin Olive Oil (EVOO) are often not extra virgin (first press) and often not 100% olive. Choosing organic olive oil is a higher price, but ensures the quality and manufacturing guaranteed by organic standards. There are no regulations in place for non-organic oils at the moment. Using liberal amounts of soybean oil or other low grade, low quality oils, especially when stored in plastic, will NOT have the same beneficial properties like polyphenol antioxidants that real olive oil has. When I was recently in Spain, a good quality bottle of organic olive oil was about 15-20 Euros. I saw the same bottle of organic Spanish oil that I brought home from Spain in Williams-Sonoma this past weekend for $25 US. This is about the price that a liter or more of high quality extra virgin olive oil goes for (unless you find some on sale.) If you are paying significantly less, you are probably getting adulterated oils.
A note on olive oil. Americans spend about 700 million dollars on olive oil per year. Low grade olive oil is rampant, and many cheap versions are cut with soybean oil or other inferior vegetable oils. Products branded as Extra Virgin Olive Oil (EVOO) are often not extra virgin (first press) and often not 100% olive. Choosing organic olive oil is a higher price, but ensures the quality and manufacturing guaranteed by organic standards. There are no regulations in place for non-organic oils at the moment. Using liberal amounts of soybean oil or other low grade, low quality oils, especially when stored in plastic, will NOT have the same beneficial properties like polyphenol antioxidants that real olive oil has. When I was recently in Spain, a good quality bottle of organic olive oil was about 15-20 Euros. I saw the same bottle of organic Spanish oil that I brought home from Spain in Williams-Sonoma this past weekend for $25 US. This is about the price that a liter or more of high quality extra virgin olive oil goes for (unless you find some on sale.) If you are paying significantly less, you are probably getting adulterated oils.
Consider shopping at an olive oil specialty store that lets you taste before you buy ~ Le Roux in Portland, Maine offers this option plus delicious balsamic vinegars to pair it with! Buying olive oil in larger amounts, like the metal cans sold at Italian grocery stores, often allows for improved quality and a lower volume price. Transfer some of the oil into a smaller table-friendly vessel for cooking and dressing raw greens! Read More about Olive Oil’s dark side.
References:
http://www.medscape.com/viewarticle/502409_5
http://www.ncbi.nlm.nih.gov/pubmed/24050803
http://www.medscape.com/viewarticle/504600
http://www.medscape.com/viewarticle/750564#vp_2
http://www.medscape.com/viewarticle/785895#vp_2
http://oldwayspt.org/resources/heritage-pyramids/mediterranean-diet-pyramid/traditional-med-diet
http://www.ciaprochef.com/northarvest/mediterranean.html
http://www.today.com/health/live-100-sardinias-secrets-longevity-blue-zones-2D80590693
https://www.bluezones.com/