Uric acid is a waste product normally present in the blood as a result of the breakdown of purines. Excessive amounts of uric acid can cause crystals to form in the joints, leading to gout. Therefore, a low purine diet will lengthen the time between flare-ups and reduce their severity.
Foods to be eliminated: most fish and seafood, all organ meats and gravy. The following foods are moderately high in purines are to be mostly eliminated. These may be eaten once a month at most:
• anchovies
• lamb
• veal
• bacon
• liver
• salmon
• turkey
• haddock * (once a week due to high omega fat content and local fish )
Some vegetarian foods have been linked to higher purine content and are to be avoided on a daily basis including oatmeal, mushrooms, spinach, beans and lentils. These may be eaten maximum once a week.
Foods to include in your diet that are known to counteract the production of uric acid include: cherries, apples, strawberries, blueberries, kale, celery, squash, watercress and avocado.
You will need to increase vegetarian sources of protein – nuts, seeds, avocado, quinoa, and eggs. I recommend 1 cup of whole grains daily (see alternative Grains handout,) a variety of vegetables, fresh fruits, and moderate amounts of dairy products including those sourced from sheep and goat . Also, protein shakes with 2 tbsp of flax oil, fresh/frozen fruit and almond or rice milk or water are beneficial. I like the RAW Protien brand shakes, although plain whey is acceptable. Go to your local health food or whole foods store, buy a number of single serving shakes, and find one you like. Protein shakes are best for post-exercise consumption for muscle gain, or as an easy breakfast.
Once a daily balance of non-purine foods has been incorporated into your lifestyle, begin working on alkalinizing your body’s pH to achieve the optimal acid-alkaline state of health.
Black cherry juice concentrate is well known to counteract gout. Drink 1 cup daily. 8 glasses of water are also required or 1.5 Liters. Also beneficial are nettle or red clover tea, and clover sprouts. Increase turmeric in cooking.
Tag Archives: medicine
Pronouns et al
I had the good fortune to be profiled in Society for Hospital Medicine’s LGBT postings this June 2023 as part of Pride Month. I was interviewed early in the Spring and received a preview of the article. The journalist stated that I did pronoun advocacy work and received the Diversity and Equity Award for my Residency class for pronoun work in the EMR. This is not true. The language from the first draft shifted just enough in the final version to have a different meaning. When I saw it in print I became VERY uncomfortable with the inaccuracy. I did not remember that point in the draft. I went back to the email exchange and indeed it was there from the beginning. It is strangely ironic that I would be highlighted as the pronoun advocate in medicine because of the very real pain that I have caused other people by mis-pronouning and misgendering them.
Although I have been involved in trans health advocacy since 2003 I have made many mistakes over the past two decades. In 2013 I gave a talk at the Philadelphia Health Conference that was disastrous; I horribly publicly misgendered several people when calling on them for questions. In 2021 I dated someone that had several GenZ friends who used they/them pronouns and we all struggled with my default to binary pronouns in unthinking moments. Therefore, to have me championed as a pronoun advocate is more bitter than sweet.
I do prefer the gender affirming pronouns of they/themme for myself. I only allowed myself to come into these pronouns in 2021 after over a year (decade) of introspection and examination. The above GenZ folks as well as social media sites like @seedingsovereignty on Instagram helped me realize that even though I have lived most of my GenX life without language to describe my gender I am free to use whatever pronouns that feel most comfortable. I have them in my work signature but I have not pushed for them personally.
The Trans health work that I do includes peer to peer level discussions about language in documentation as many health care providers still use language from the 1990s. I provide trauma informed care for my patients of all genders, and have a special place in my heart for all gender nonconforming folks in health care settings. I work with administrative staff, creating education about the gender spectrum and experience of gender and sexual diverse individuals to create safe medical homes for LGBTTIQ2S folks. And, moving forward I am working to create Justice/Equity/Diversity/Inclusion community gatherings within internal Medicine to lift the voices of Black, Indigenous and Trans physicians towards leadership roles as these are the least represented identities in medicine (and therefore the most needed.)

Notes from the Road: Buenos Aires WPATH
I am in beautiful Buenos Aires at my second World Professional Association for Transgender Health. My first was held in Amsterdam in 2016 when I was a fresh faced, just-finished first year medical student. Now, as a mid-fourth year student I am significantly more exhausted and disillusioned; I also have so much more doubt about choosing this field of medicine as my calling.
I like to tell the story that I returned to medical school to practice transgender health. Specifically, to be able to prescribe transitional hormones and participate in the insurance racket to reach more people. And that is part of the story. The root truth is I have been compelled to be a full scope physician for many reasons and transgender medicine gave me a focus because it was something I could not attain as the Naturopathic Doctor that I was before.
 The last session I attended at the WPATH ARGENTINA conference was an incredible and inspired panel of Brazilian intellectuals speaking on depathologizing the transfeminine and deconstructing cisheteronormativity. Fran Demetrio, a transfeminine Brazilian professor was so passionate and eloquent in her discussion of injustice, oppression, systemic violence and the colonization of knowledge imported by biomedicine. She was being translated which made some of the discourse hard to fully comprehend and I wished WPATH had provided a professional translator for her because what she had to say was so profound and important and well thought out. She framed a paradigm that took the personal out of the conversation and raised it to a social construct and human justice level. In rough translation, she explained that not including the existential experience of trans voices in episystemic medical knowledge creates symbolic violence and perpetrates the colonialism of transgender relationships. This generates mental health violence and tramples the [transgender] patients knowledge. Considering and understanding this is essential to depatholgize the trans experience.
The last session I attended at the WPATH ARGENTINA conference was an incredible and inspired panel of Brazilian intellectuals speaking on depathologizing the transfeminine and deconstructing cisheteronormativity. Fran Demetrio, a transfeminine Brazilian professor was so passionate and eloquent in her discussion of injustice, oppression, systemic violence and the colonization of knowledge imported by biomedicine. She was being translated which made some of the discourse hard to fully comprehend and I wished WPATH had provided a professional translator for her because what she had to say was so profound and important and well thought out. She framed a paradigm that took the personal out of the conversation and raised it to a social construct and human justice level. In rough translation, she explained that not including the existential experience of trans voices in episystemic medical knowledge creates symbolic violence and perpetrates the colonialism of transgender relationships. This generates mental health violence and tramples the [transgender] patients knowledge. Considering and understanding this is essential to depatholgize the trans experience.
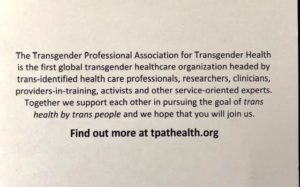
Despite the multiple disparities that this population faces world wide, there is a slowly increasing body of trans identified physicians and health leaders in the field. However, to date many of the people making the decisions about gender medicine are not differently-gendered themselves. Surely, this is problematic. The numbers of trans identified health care leaders is increasing by the year, and with groups like the Transgender Professional Association for Transgender Health, they are seeking greater control around the discourse of gender medicine and claiming their place as necessary voices in the didactic. 
The tensions between cis and trans leadership has created a simmering anger within this medical community. A socialist friend of mine shared that in activism in general there is a current trend towards challenging aggressions towards advocacy leaders in many different fields with a similar theme of – who has the power to speak and represent the cause?
 I was personally attacked in this rising conflict this year when I created a transgender health elective as a third year medical student for global medical students to supplement core medical school curriculum. A variety of trans and nonbinary people on social media threatened to create a petition against the course as it does not have a transgender identified course leader and there were multiple flamings on Facebook. I personally received several vitriolic emails from different people about the course, its content, and my leadership. I was privileged to have a team of (cis and transgender) people who have been in the field for a long time holding leadership positions to assist me in creating online and email responses that were balanced, appealed to reason, and illustrated the many ways the course seeks to uphold and respect the “nothing about us without us” principle while promoting evidence based foundational medicine.
I was personally attacked in this rising conflict this year when I created a transgender health elective as a third year medical student for global medical students to supplement core medical school curriculum. A variety of trans and nonbinary people on social media threatened to create a petition against the course as it does not have a transgender identified course leader and there were multiple flamings on Facebook. I personally received several vitriolic emails from different people about the course, its content, and my leadership. I was privileged to have a team of (cis and transgender) people who have been in the field for a long time holding leadership positions to assist me in creating online and email responses that were balanced, appealed to reason, and illustrated the many ways the course seeks to uphold and respect the “nothing about us without us” principle while promoting evidence based foundational medicine.
I brought up this conflict between cis and trans leadership in the didactic of transgender medicine again at one of the ethics seminars at WPATH, where leadership and authority privilege was being discussed. Unfortunately, I was emotional in my questioning of the ethics behind attacking ally’s and advocates, as I am still deeply shaken by this experience. The response from one of the panelists was that when working as a non trans person with the gender diverse community there is so much anger one must simply expect to be attacked and be ok with that.
I am a person who has been excavating emotional violence in my personal life and creating real boundaries to protect myself for the first time. I don’t think I can intentionally choose a career were the population I am exhausting myself to serve reserves the right to be emotionally violent towards me indiscriminately because of their experience of violence. That is like saying that my mother has the right to be violent towards me in any way she sees fit because of the abuse she and her mother suffered. No.
Again.
“not including the existential experience of trans voices in episystemic medical knowledge creates symbolic violence and perpetrates the colonialism of transgender relationships. This generates mental health violence and tramples the patients knowledge. Considering and understanding this is essential to depatholgize the trans experience. “
Dr. Demetrio’s message ultimately lifted my perspective of the conflict to a healing systems approach. With this in mind, I am still recalibrating my commitment to trans health as a specialized field of medicine, while intentionally making room for the many trans identified health care leaders. As a nontrans woman and a white queer/lesbian, I devote the next phase of my medical education to the foundations of internal medicine as well as lesbian health, vaginal happiness, fertility, community health, and queer health issues like addiction and mental health. My view of women’s health includes trans and cis women, as does my passion for community wellness. I am confident that these past 11 years of studying transgender medicine and advocacy work will continue to inform the communities I serve, if in a less direct way.
I see now that when I claim my leadership vision within a paradigm that matches my own identity I can be stronger and more authentic.
Embedding Resilience in Medicine
 Half an inch from the first four thoracic vertebrae lie the central nervous system transistors (stellate ganglion) for your fight and flight nervous system. Needless to say, my upper back is constantly aching. I am metabolizing the unique stress of being a brand new doctor/medical student in hospital life. It’s a different kind of stress than the first two academic years: those were crushing content & exams, but they were ivory tower academia. This is the very real medicine that is literally birth, life and death stuff. More visceral than literal, I find myself often crying, sometimes gagging, and occasionally elated.
Half an inch from the first four thoracic vertebrae lie the central nervous system transistors (stellate ganglion) for your fight and flight nervous system. Needless to say, my upper back is constantly aching. I am metabolizing the unique stress of being a brand new doctor/medical student in hospital life. It’s a different kind of stress than the first two academic years: those were crushing content & exams, but they were ivory tower academia. This is the very real medicine that is literally birth, life and death stuff. More visceral than literal, I find myself often crying, sometimes gagging, and occasionally elated.
The purpose of third year clerkship aka #MS3 is to get a sampling of each major specialty to help us decide on a residency. Its a generic med school formula consisting of: Pediatrics, Surgery, OB/GYN, Internal Medicine Inpatient & Outpatient, Family Medicine, Psychiatry, Community Health. Inpatient, we legally cannot write patient notes. While we can actively participate in patient care, everything we do needs to be seconded by a licensed doc; therefore, we are mostly shadows, errand runners, and absorbent sponges.
Unfortunately, some throwbacks to fraternal physician hazing rituals are still in place even for third year medical students. For example, my Internal Medicine inpatient rotation, which is already a 6am – 6pm shift 5 days a week (with a 1 hr drive on each side) also requires 6 -24 hour shifts in the 6 weeks. I asked a friend who is a year ahead of me and attended a different hospital clerkship if her rotation was scheduled as such, and she said she had to follow hospitalist hours for that same rotation – roughly 730am – 330pm. If the point is to learn each of the specialty’s roles, it makes sense to follow the professional hours. If the goal is to teach us that Internal Medicine requires an exhausting slog of hospital life, and how to forsake all other aspects of our personal and academic life for our career, then this approach in third year makes sense. Slate Magazine said it best: Third Year Kills Humanity of Medicine.
I haven’t done the above inpatient IM rotation yet and yes, I’m actively worried about my health, my marriage, and my coping skills during that onslaught. I did one 86 hour “sneak peek” week with our Family Medicine inpatient service last Fall. I did enjoy the steep learning curve and patient contact; however, I often felt lost and useless as my resident dictated her many notes and ran around the hospital following up on pages and other details. I did get some good studying done and learned some basic inpatient skills but there were hours, especially after the first 8, that I wished I had something more productive I could be doing in.
In reality, the residents are much more forgiving than the administration and often let us leave early (6am – 10/11pm) saying “there is nothing we could learn at 2am that cant be learned at 2pm.” I am eternally grateful for this ray of grace. And I do understand that night shifts and on-call hours are foundational for many physician careers and practicing them could be relevant. But why, when 55% of Internal Medicine and Family Doctors report burnout, are we being subjected to these mind numbing hours as third years? How will medicine ever change if the hazing continues to be perpetrated generation after generation?
I accept that being a doctor requires selflessness & sacrifice. I accept that long hours are often required and I like to work – for an income, for a team, and for a good reason. I’m a second career medical student, I study and practice clinical skills because this is what I love! I accept that as a resident I will bear the brunt of hours spent watchdogging and admitting in part because we are the cheap labor force of institutionalized medicine. But, I have 1.5 years of med school left, and 3-6 years of residency/fellowship ahead. What is the purpose of having me work 86 hour weeks now, and how is it going to benefit my relationship towards medicine?
 To embed resilience in doctors, we as a profession and as an academic incubator need to provide time & space for rest, relaxation, and quietude. Only in parasympathetics can we metabolize the soul-rattling experience that comes from facing death and sickness and the burden of chronic disease in North America. Not only are we facing grief/loss/mortality, we are taking on the enormous responsibility of decision maker. A backlog of unprocessed emotion leads to substance abuse, chronic pain, sleep disorders, lack of compassion, and who knows what other organic & chemical dysregulation. We need regular daily time to cook good food, sleep with our loves, be intimate and vulnerable, Netflick and chill, get to the gym or get outside. Only in that space can we emotionally integrate this transformation.
To embed resilience in doctors, we as a profession and as an academic incubator need to provide time & space for rest, relaxation, and quietude. Only in parasympathetics can we metabolize the soul-rattling experience that comes from facing death and sickness and the burden of chronic disease in North America. Not only are we facing grief/loss/mortality, we are taking on the enormous responsibility of decision maker. A backlog of unprocessed emotion leads to substance abuse, chronic pain, sleep disorders, lack of compassion, and who knows what other organic & chemical dysregulation. We need regular daily time to cook good food, sleep with our loves, be intimate and vulnerable, Netflick and chill, get to the gym or get outside. Only in that space can we emotionally integrate this transformation.
Our clerkship Dean Dr. Taylor sent out this reaffirming blogpost last month in which an experienced physician Dr. Youngson writes to his younger self. He says:
“As a medical student or junior doctor, it’s easy to feel powerless especially in a hierarchical medical system that too often teaches by humiliation, punishes those who question the status quo, and grinds people down through overwork and inhuman working conditions…”
Change medical education so that we as medical students (and residents and attendings and all doctors actually) are seen as people who are more than life-saving, problem fixing, chart dictating, disease curing machines. A more gentle, humane practice of time & space for medicine while living life alongside the role of physician has to start at the beginning of the clerkship year when we integrate it’s practice with our academic foundations, or it wont be ingrained as part of the way we approach medicine.
Once I started thinking about time, resilience and integration as the cure of medical burnout, I began seeing evidence everywhere. I heard a NEJM Interview from 01/03/18 with Dr. Armstrong from Massachusettes General Hospital’s new Pathways program where residents are given time and a scientific team to investigate complex patient-based cases. The 12/26/17 issue of JAMA has an article by Jack Coulehan, MD MPH from the Center for Medical Humanities, Compassionate Care and Bioethics on Negative Capability and the Art of Medicine that speaks to “sustaining the physician through the ‘humdrum routine’ of professional life… [Using]… the power to recognize the ‘true poetry of life'” and of medicine. This is a reflective practice. He says:
“In pursuing the steadiness and detachment required to master clinical practice, it is tempting to neglect the more difficult project of nourishing engagement and tenderness in our relationships with patients – and with ourselves.”
The future of medical education is not only about competencies met and clinical acumen. The true scholars of the next generations of physicians will be those who can achieve their best in patient care and scientific fulfillment, while also living a satisfying, integrated and joyful life.
Evolutionary Success vs Child Free Living
As you know, I have been struggling with my biological clock: my age and stress level tick louder than ever. Weighing the cost of motherhood against my career in medicine has never been an equal balance with scales always tipped in the favor of my seemingly insatiable appetite for knowledge. And yet – I’ve been studying fertility since 2004, seeing fertility docs since 2008, and froze my eggs in 2013. I am always scheming to figure out “when is a good enough time”. Yes, I know there “is never a good time: but as a lesbian with a choice, isnt there a “better time”? And here I am, child free, finally happily coupled, and in my third year of medical school in 2017.
I just completed 6 weeks working with newborns and doing well-baby checks to mostly women under 30 in my first pediatric rotation. I I couldn’t help thinking about the definition of evolutionary success as progeny. Many moms I worked with had 4-8 other babies. Some were on opioids, many smoked pot and tobacco or even took buspirone and SSRIs throughout their pregnancy and had sick/addicted babies. Some were very very young. But evolutionarily, each of them had already surpassed me even with my 2.5 degrees, $500k of education, and diverse, privileged, happy life. I realized I am currently an evolutionary failure.
 I am an archetype of my Generation X. I don’t have many excuses for child-free living left, having had a bacchanalian and free-spirited 20’s and 30’s. Is it time for me to “settledown”? Who am I if I choose NOT to have a child of my own?
I am an archetype of my Generation X. I don’t have many excuses for child-free living left, having had a bacchanalian and free-spirited 20’s and 30’s. Is it time for me to “settledown”? Who am I if I choose NOT to have a child of my own?
My primary reasoning for not spawning includes RESPONSIBILITY – towards my career/education and more importantly, to the kid. Who brings a child into the world who is guaranteed a mom who is away from home 12-18 hours a day (unavoidable in medical school -residency)? Where is the evolutionary success in that? Generationally, I do not have the same programming my parents had to marry/reproduce, and as a lesbian it didn’t happen by accident. Also, as a kid myself who had a high ACE score, I don’t want to perpetrate even a privileged neglect into another generation. So, here I am: struggling with my generational expectation to break the glass ceiling, achieve my highest ambitions, follow my dreams … and shouldering the unspoken price of doing that.
Maybe I could redefine evolutionary success. Not “survival of the species” but survival of the…planet? Conscious eco-systeming? Or maybe even the more complicated redefining of family/familial success – what if evolutionary success was a life well-lived and well-loved, and a small carbon footprint; a kinship network of peers, lovers, and lifelong friends instead? Children no longer live to serve their elder parents, and even if I had a child, I would not be promised a safe and well-cared for death. Still, at the end of the day, even though I have many cousins with beautiful babies carrying on the family line in all directions, my personal lineage of Wright-Larson will not be carried on unless I have a kid. That feels sad. That does feel like failure.
I stand with my aching feet and my scrubs and pager, knowing raising my own babies is not likely going to be the life I get to live this time around.
I have always been an outlier. I chose Naturopathic medical school in the 90s, chose the urban underbelly in the 2000s, and chose osteopathic medical school in the 20-teens. I’m 92% reconciled that I will enjoy my child-free life and travel to Tokyo, Vatican City, Barcelona, and live in expensive, romantic urban centers. Because I consistently choose career, love and adventure over a baby and domesticity I will be able to live a certain kind of lifestyle. But that doesn’t make it easier when I come home smelling like babies from a day at work, or when I see my cousins achingly beautiful creative charming kids. There is no consolation prize for evolutionary failure. Only the small faith that I am making the right choice for the kid I would create and maybe a for this planet, and hopefully for, myself and my love.
(Least)* Complicated
Walking the tightrope between being a current MSII medical student and a Naturopathic Doctor is a delicate balance sometimes. I never know whether my career as an expert in alternative medicine is going to be a blackball or a gold star because of the very mixed opinions people have about my former profession in the medical world. My plan, heading into the first day of medical school was not to tell anyone my (second) degree when I started (my third degree) at UNECOM, but it was announced in orientation so my cover was blown.
Being a ND in general is pretty complicated – working outside of insurance in most states is a financial challenge for patients as well as doctors, and public knowledge about the profession is highest on the west coast of the US and Canada, and in more affluent areas of the NorthEast. Many people get excited when I say I am a doctor, then look back blankly when I tell them what kind of medicine I practice(d). People who know the field have reactions that are pretty love: hate. Lots of lovers, quite a few haters, and an ever-growing population of quiet converts who realize that, as one anonymous Twitter medical student said in my recent Twitter Flaming on the topic: people who are interested in alternative medicine are usually trying to take care of their health and make themselves feel better.
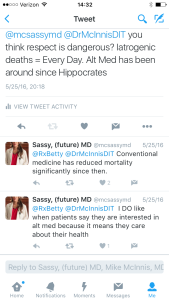 I have recently been made aware of a woman who attended a west coast Naturopathic Medicine College who has turned against the profession “with an inside view” and who is engaging in aggressive muckraking. She is getting recognition and validation as an “insider” to Naturopathic Medicine as she did complete our 4-year postgraduate degree before she quit and moved to Germany. She has started a petition to defame the profession worldwide. The unfortunate thing is she lives outside the US and is not accountable for US or CDN slander laws. What she is doing is poignantly effective because she has inflamed the haters. One doctor in particular is a physician and educator with the influential Doctors in Training Boards Exam Review Series. He has a large Twitter following and has enthusiastically joined in the slander of the Naturopathic Profession. I worry about how his “expert” personal opinion will effect future generations of physicians who have not considered their professional opinions of Naturopathic Medicine due to lack of exposure.
I have recently been made aware of a woman who attended a west coast Naturopathic Medicine College who has turned against the profession “with an inside view” and who is engaging in aggressive muckraking. She is getting recognition and validation as an “insider” to Naturopathic Medicine as she did complete our 4-year postgraduate degree before she quit and moved to Germany. She has started a petition to defame the profession worldwide. The unfortunate thing is she lives outside the US and is not accountable for US or CDN slander laws. What she is doing is poignantly effective because she has inflamed the haters. One doctor in particular is a physician and educator with the influential Doctors in Training Boards Exam Review Series. He has a large Twitter following and has enthusiastically joined in the slander of the Naturopathic Profession. I worry about how his “expert” personal opinion will effect future generations of physicians who have not considered their professional opinions of Naturopathic Medicine due to lack of exposure.
Big media like Forbes has jumped on the “tin foil hat” bandwagon by supporting her claims that botanical medicine, nutrition, physical medicine, homeopathy, mind/body practices and stress management are invalid sciences without evidence. The American and Canadian federal Naturopathic associations have both started a counter-petition against these muckracking efforts.
All of this is personally upsetting for me. It stirs a complicated turmoil of emotions, injustice, pride, and frustration that mixes my own choices with a very clear working knowledge of the weight that “the big lie” technique can carry in the world of propaganda. All of this comes at a time when “Functional Medicine” and “Integrative Medicine” are the new darlings of allopathic medicine alongside epigenetics and the microbiome.
Newsflash: Functional Medicine and Integrative Medicine ARE evidence based Naturopathic Medicines, researched by and for NDs originally.
Naturopathic Doctors are systematically being defamed and slandered while our actual practice techniques are being picked up and renamed and celebrated for their effectiveness.
I feel helpless in the face of this complicated adversity. I made my personal choice to add an Osteopathic Degree to my knowledge base because there was more to medicine I wanted to know – pharmacology, emergency medicine, psychiatry, and other facets of transgender medicine I need additional training on. I know the great value of Naturopathic Medicine and so do a great number of North American consumers. I suppose I need to trust that the greater good will prevail in the end…. but that may not help me or my career path when I am placed in a hospital as an MSIII or resident with an attending like the Internist above who hates everything alternative and Naturopathic medicine stands for.
The Lost Art
I am sick in an invisible way that people cant really see, and I don’t really feel – much. I can take a pill and make it mostly unnoticeable. Except for the fact that my hair falls out in handfuls with a certain kind of stress…
I consider myself an expert in self-care. And yet, I can hardly find the time to do the “little” things that I know could help. Like, nettle hair rinses, getting at least 8 hours of sleep every night, taking my fish oil, and eating more protein. Instead, I keep myself too busy and dull myself with things that make me feel better for a few hours, but never in the long run. I have fallen into the mindlessness of modern health care where I want a pill to do the work of healing for me. Dammit!
We all have levels of health maintenance we are willing to do on a regular basis. Vitamins, exercise, water, organics, therapy, whatever. We each have a certain degree of self care required to maintain the status quo of daily function. But, what happens when that balance is tipped and we need to actually recover from an illness, injury, or accident?
I offer you an invitation to step off the rat wheel of everyday living, and create a luminal space for healing. A luminal space is an anthropology term that refers to a period of time “outside of time” – a step out of everyday living. Some health crisis force this through body fluid effluvia that ties one to the bathroom, or physical disability that prevents mobility. Too often we are able to power through a cold, or anxiety attack or injury and do not engage in the art of self care to allow actual healing. This is what snowballs into chronic illness / disease or chronic pain.
I have been “sick” for at least 9 months, but I haven’t made more than a few half-hearted efforts to engage in deep self care. I have taken lots of prescriptions and had lots of blood tests, but is that truly healing medicine? I finally broke my baby toe last week, and have been suddenly forced to slow down by immobility. I am doing hydrotherapy, making castor oil packs, cooking and eating good food, meditating, saying no to social engagements I don’t deeply want to do, and getting sleep. These are some of the cornerstones of deep self care.
It is very difficult to give ones self approval to close the door on society and expectations and family, and friends, and chores, and domestic duties, and distractions, and choose to do something solely for the self instead. We are culturally programmed to take care of business, pleasure, family, kids, dogs, and our homes before we take care of the inner self. If you are sick, at any level, you will heal faster, and better if you take the time to practice deep medicine by taking the time to take care of your self.
I am here to help you do that. And, I give myself permission to offer that same wisdom and practice for my self. The pills and the maintenance are not enough. We must engage the luminal, lost art of deep self care for complete health and healing.
Counter-Response to the Multivitamin Controversy
This post was originally written for Apothecary By Design in December 2013 http://www.apothecarybydesign.com/blog/
Stop Wasting Money on Vitamin and Mineral Supplements! 5 medical doctors cried out in an editorial piece first released in the Annals of Internal Medicine, and then circulated through all major newspapers and social media outlets early this week. The articles released in the New York Times, Wall Street Journal, LA Times, and countless other newspapers pointed out that multivitamins have failed to show benefit in several large scale studies; however, the evidence reviewed was not as clear as we were led to believe. As with every evidence based study, it is important to look at the information behind the research, the studies cited, and the actual information the studies gathered.
The quality of multivitamins IS a true concern for consumers. The studies supporting multivitamins have been mixed, and we acknowledge this. If you are going to take a multivitamin it is not an effective use of money to buy a low quality product (like the one illustrated below) that is not well absorbed and/or is coated in toxic chemicals and fillers. A very good diet may reduce or eliminate the need for a daily dose of essential nutrients. Some multivitamins may be a waste of money, not because studies illustrate a lack of benefit, but because of the abysmal quality of the product itself. Choosing an appropriate multivitamin is another question – one that Apothecary by Design’s wellness specialists welcome.
The following studies were used to support the evidence that multivitamins are not worth taking:
 1. Multivitamins and cognitive decline in men 65 or older
1. Multivitamins and cognitive decline in men 65 or older
For example, in the first study on cognition, the multivitamin assessed was a well-known common multivitamin that provides low level nutrients in the cheapest, least bioavailable forms. These poor quality minerals generally include oxides and sulphates. For example, magnesium sulfate is epsom salt, like you would use in a bath. Magnesium citrate is a better quality, more absorbable mineral. (See label) Check out the “other ingredients” as well – 3 artificial colors including the noxious FD&C Red #40.
Regardless of the supplement quality, cognition issues are not primarily related to vitamin/ mineral deficiencies, but are a long term response to heavy metal toxicity, poor cerebral perfusion (not enough blood to the brain), omega 3 deficiency, hormone deficiency, environmental contamination, stress and elevated cortisol levels, head trauma, prescription medication side effects and many more individual variants.
For example, how many of the physicians studied were also taking statin drugs? These ubiquitous prescription medications are known to have memory impairment, loss of memory and amnesia as potential side effects.
When presenting strong statements like multivitamins are a waste of money, it is responsible to use evidence that considers a straighter line between cause and effect.
2. Multivitamins failed to reduce cardiovascular events in men and women with previous myocardial infarction
The second study cited as proof that multivitamins are a waste of money was a 2012 study evaluating the effects of chelation therapy on men and women over 65 with history of a heart attack.
This study had significant setbacks. Chief among them were the high drop-out rates due to the strenuous protocol of 30 weekly chemical chelation infusions followed by 10 maintenance infusions two to eight weeks apart.
It is difficult to assess the effect of a multivitamin on long term health with such invasive chemical and vitamin therapies being administered at the same time, and it certainly clouds what is presented as a black and white result.
Antioxidants, nutritional counseling and botanical therapies are also first line treatments in the Integrative health world to repair myocardial function. Once again, the true nature of the study being cited is obscured by the dramatic headlines.
2. Multivitamins did not prevent the development of chronic disease or death.
If only a simple, cheap, low dose, poor quality multivitamins could save the world from chronic disease….
Quality matters in the food we eat, the medications we take and the supplements we buy. Chronic disease is a complex, multifactorial health concern whose cure cannot be reduced to oversimplified statements like these.
Finally – the original article states “….beta carotene, vitamin E and possible high dose vitamin A supplements increase mortality.” What they leave out, is that high dose beta-carotene increases risk of … lung cancer in smokers (only.) And alpha-tocopherol vitamin E increases the risk of heart disease …but full spectrum vitamin E with both tocopherols and tocotrienols reduce the risk. Limiting the information sensationalizes the story, obscures the evidence and limits its relevance.
The great thing about this editorial is that it exposes the poor quality multivitamins out there for what they can be: a sense of false security. No one can eat fast food regularly, take a poor quality low dose multivitamin, not practice any preventative measures, and not develop chronic disease eventually. That much IS true.
A multivitamin needs to be able to be absorbed, with high quality minerals and therapeutic dosages of vitamins at the very least to offer prevention and protection. These remain a worthwhile investment for people wanting to maximize their nutritional value. Furthermore, high quality children’s multivitamins remain a good nutritional adjunct for picky eaters and kids with behavioral or health issues. Multivitamins are not a substitute for a healthy lifestyle with good quality food choices, exercise, and stress reduction.
http://www.mayoclinic.org/medicalprofs/trial-to-assess-chelation-therapy-cvuv10n4.html
http://www.ncbi.nlm.nih.gov/pubmed/10359235
http://www.medscape.org/viewarticle/501471
Enough Is Enough: Stop Wasting Money on Vitamin and Mineral Supplements. Annals of Internal Medicine. Eliseo Guallar, MD, DrPH; Saverio Stranges, MD, PhD; Cynthia Mulrow, MD, MSc, Senior Deputy Editor; Lawrence J. Appel, MD, MPH; and Edgar R. Miller III, MD, Phd p. 850
September 2013
 Apples are in season again, so it must be time to go back to school. This year, I will be the one in front of the classroom! This is completely new for me, and I have been anxiously preparing mentally (and literally) for most of the summer. Academics are an important part of a doctors CV, and an area that I have studiously avoided in my career thus far. But when Corinne Martin at University of Southern Maine Nursing School contacted me about the program she has been developing as a holistic health minor for USM the fear was less than the excitement. I am honored to be teaching CON 284 Botanical Therapies for the fall semester. The course is an introductory level exploration some of the issues that surround medicinal plant use including historical dynamics, ecological effects and cultural perceptions of herbs. I will also be teaching practical clinical use of commonly used botanicals. We have guest speakers coming in, a practical how-to workshop on medicinal preparations, and a diverse reading list. Plant medicine has been foundational to my practice, and I am grateful for the opportunity to expand my own understanding and become more of a community resource!
Apples are in season again, so it must be time to go back to school. This year, I will be the one in front of the classroom! This is completely new for me, and I have been anxiously preparing mentally (and literally) for most of the summer. Academics are an important part of a doctors CV, and an area that I have studiously avoided in my career thus far. But when Corinne Martin at University of Southern Maine Nursing School contacted me about the program she has been developing as a holistic health minor for USM the fear was less than the excitement. I am honored to be teaching CON 284 Botanical Therapies for the fall semester. The course is an introductory level exploration some of the issues that surround medicinal plant use including historical dynamics, ecological effects and cultural perceptions of herbs. I will also be teaching practical clinical use of commonly used botanicals. We have guest speakers coming in, a practical how-to workshop on medicinal preparations, and a diverse reading list. Plant medicine has been foundational to my practice, and I am grateful for the opportunity to expand my own understanding and become more of a community resource!
I work primarily at the Age Management Center these days, with a strong focus on hormone health. I work with Dr. Michael Bedecs who is a Men’s Health expert, and is extremely experienced in hormone replacement. I am grateful to say he has taken me under his wing, and I have found a permanent place for my private practice here in Maine (and beyond.) It took almost two years to find the right work environment and business associate after owning my own clinic for 11 years in Toronto. Stay tuned for new articles on fertility, perimenopause and transgender/transsexual health care. When working with hormones, it is impossible not to consider trans* health care, as this is a population often dependent on hormone use. Dr. Bedecs and I will continue to merge his extensive knowledge of hormone use with my specific integrative medicine training, community commitment, and health care activism to create a concierge style medical practice to serve all genders equally with cutting edge comprehensive treatment plans.
The other work I have been doing is more personal, learning how to trust my gut. Who is good at this? Tips? Strategies? It is so hard in this mixed modern world for me to be able to sift through the messages that come from outside vs. those that come from inside. What I have learned, is that if the inner messages are not heeded, outside havoc will soon result. Or, an event will occur with a big “I Told You So” tag on it. This is part of my process as a human – what is your process? We all have evolutionary issues that we work though, each as unique as stars. Having good guides – as partners, therapists, teachers, doctors, friends – is key to actually learning from our process and not repeating the same mistakes. I am lucky to have all of the above right now – except a good Dr. That is next on my list!
Thank you for reading through, for listening. My health story is mirrored in my life, and I know all of yours are too. It is the details of life that illustrate the pathways of disease and also those of health. Find yourself a Dr that will listen for the details, and trace paths. Take a new course. Call someone you miss. Step outside your comfort zone and do something professionally that scares you! It is September 2013, the time is ripe!
Nutrition, Herbal Medicine, Homeopathy
Naturopathic medicine is not a single kind of healing, but is an array of healing practices. I think of Naturopathic Medicine as a wheel, and what we do as the different spokes that make up the whole. These “spokes” are called modalities, and include acupuncture, counseling, herbal medicine, functional medicine, homeopathy, massage, minor surgery, nutrition and in some states/provinces, prescription medications and/or IV therapies. Naturopathic Medicine is diverse – each doctor chooses what areas to focus on. Many N.D.’s choose one specific modality, like acupuncture, functional medicine, or homeopathy. Others, like myself, are eclectic and utilize many of the modalities, depending on the individual case.
Acupuncture, counseling and massage are not as applicable for self care; however, nutrition, herbal medicine, and homeopathy are very important ways that people can take care of themselves. There is only so much help that Dr. Google can offer. If general information basics are not resolving the issue, or you have complex health concerns with multiple medications involved, having a licensed ND assist you in recovery is going to be the most effective and safest utilization of natural medicines.
NUTRITION is the philosophy of using food as medicine. Nutrition can be used therapeutically to treat specific conditions – such as eating beets and dandelion leaves for liver cleansing, or cabbage juice for ulcers. The foods that we eat in 2013 are very different from what our grandparents were eating. The soils are stripped of minerals (or toxic like on Munjoy Hill, ) many foods are genetically modified, and the preparation and processing of foods radically alters nutritional values. Supplementation is generally included with nutrition as it is often necessary, given today’s food choices, to supplement some nutrients that are no longer found in food.
HERBAL MEDICINE is an excellent way to treat the whole family. In theory, it is similar to using pharmaceuticals – specific components within each herb cause specific actions in the mind, body and spirit. Herbs can have a powerful action or a gentle action. Generally, the best herbs for self care are simple, common and safe for everyone in the family. If there are any specific contraindications such as interactions with medication, I would be sure to mention those. The general dose for herbal medicine for an adult is 1 teaspoon of tincture (alcohol extract) in a small amount of water, 3 times a day. Teas are drank hot 2-3 times a day or as needed. Children’s dosage can be determined as follows:
Patients weight in lb divided by 150 = percent of dose
ie) 70 lb child / 150 = 0.46 so child gets slightly less that ½ adult dose.
If is 1 tsp 3 x a day for adult, give ½ tsp 3 times a day to child.
Herbs are generally best taken on an empty stomach, to maximize absorption.
HOMEOPATHY is a very complex system of medicine that gently supports the body’s ability to heal itself through the use of “remedies” and the philosophy that “like treats (or cures) like.” The specific remedy chosen is one, which, if given to a healthy person, would elicit the very symptoms of an illness. Therefore, the remedy is known to cure that illness. Homeopathic treatment can be a profound journey of self-discovery as old wounds are healed and our true potential is illuminated. Explaining the mechanism of homeopathic medicine is difficult as it operates on the quantum level rather than the commonly understood Newtonian mechanism of action. Symptoms are seen as effective reflections of compensation on the mental, physical, and emotional levels. For example, when a warning light comes on in your car, we investigate what was wrong with the engine, not just disconnect the light! Seen as warning lights, symptoms are the body’s way of showing the outside world that something is wrong or not working properly. The constellation of symptoms points the Homeopathic Doctor to understand the bigger picture overall, and which remedy is indicated to effectively treat the underlying condition. A Naturopath practicing Homeopathy gives a homeopathic remedy to stimulate the body’s defense systems to complete the healing process. This is the concept of the vital force: the body is always trying to move towards health. This medicine is an extremely safe and effective method of eliminating disease.

